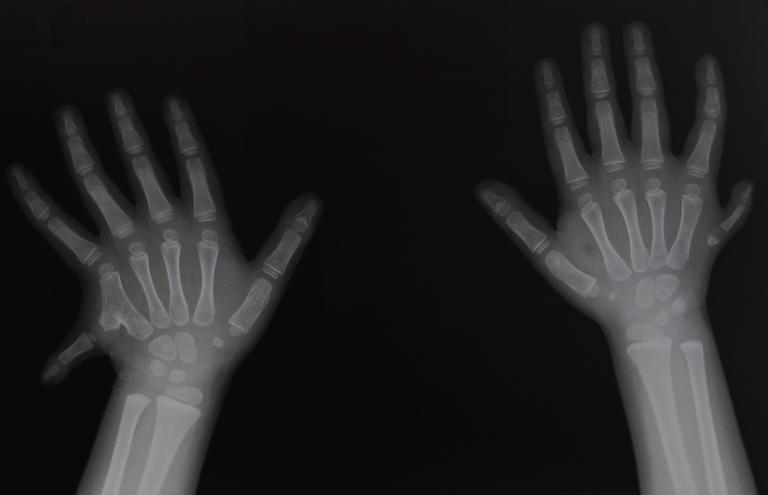
What age does my baby need to be, to have surgery?
Most extra digits on the little finger side of the hand are not fully formed digits. This may have a surgical clip placed to promote the extra digit to fall off within 1-2 weeks. A small nubbin of tissue may be the only remnant in these cases that may persist as a small mark of where the digit was removed. Excision is an alternative to clip placement and can be safely performed in the newborn period with local anaesthetic while your baby feeds/is on your breast as long as the extra digit does not have any major structural features (e.g. bones or tendons). Sometimes a small stalk of skin is all that attaches the extra digit to the hand and simple excision of this and closure with a few dissolving sutures is sufficient to remove the digit and leave very little trace that the extra finger was there.
If your baby’s extra digit involves major structural features, we will need to wait until your baby is at least four months of age, and is able to tolerate a general anaesthetic. Your RPS surgeon will advise you as to whether this is necessary.